Mate rehu ohotata iti Transient ischaemic attacks
Causes of a transient ischaemic attack
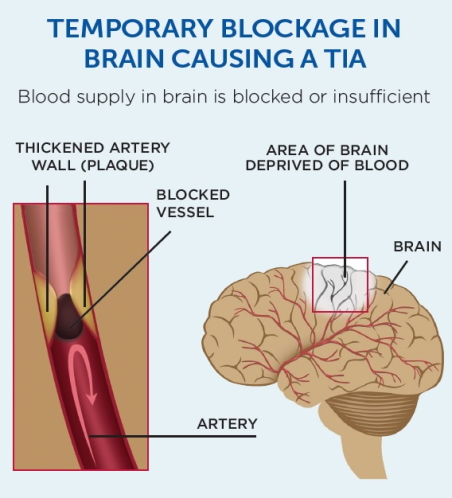
A transient ischaemic attack happens when the blood supply to part of your brain is temporarily blocked. In most cases, this is caused by a blood clot that develops because of narrowed arteries (atherosclerosis).
With a transient ischaemic attack, the blockage is temporary because the clot either dissolves or moves. After this, the blood supply to your brain returns to normal and the signs disappear.
Risk factors for transient ischaemic attack or stroke
The main risk factors for having a transient ischaemic attack or a stroke are:
- high blood pressure
- having narrowed arteries (atherosclerosis)
- the heart rhythm problem atrial fibrillation.
Doing a cardiovascular risk assessment can show if you have an increased risk of having a stroke or heart attack.
Symptoms of a transient ischaemic attack
The symptoms of a transient ischaemic attack are the same as those of a stroke. But unlike a stroke, they only last for a few seconds, minutes or hours.
The main symptoms of a stroke are known as FAST. These are:
- Face – face drooping on one side.
- Arm – arm weak on one side. The leg may also be weak.
- Speech – speech jumbled or slurred.
- Time – Time is critical. Call 111 for an ambulance.
Other less common symptoms include:
- dizziness, loss of balance or an unexplained fall
- loss of vision, sudden blurring or decreased vision in one or both eyes
- difficulty swallowing.
You may have more than one transient ischaemic attack. The signs and symptoms of each may be similar or different, depending on which area of your brain is affected.
If you think you may have previously had a transient ischaemic attack and did not get it checked out, make an appointment to see your healthcare provider.
Diagnosing a transient ischaemic attack
When you visit your healthcare provider, they will ask you questions about your symptoms and what happened and they will examine you. You may need further tests.
Tests you might need include:
- blood tests
- an ECG test to look for an irregular heart beat or other heart problems
- a CT scan of your brain
- a scan of the blood vessels in your neck.
Treating a a transient ischaemic attack
Although the symptoms of a transient ischaemic attack go away in a few minutes or hours, you will need treatment to help prevent another attack or a full stroke happening in the future.
Treatment may include:
- medication to stop clots forming (antiplatelet medication)
- medication to control blood pressure
- statin medication to lower cholesterol
- blood-thinning medication (anticoagulants) if you have atrial fibrillation.
Preventing transient ischaemic attacks
You cannot control all risk factors, but lifestyle changes can help you lower some risks. This means:
- if you smoke, stop smoking
- eat healthy food
- avoid too much alcohol
- keep active
- maintain a healthy weight.
See your healthcare provider to get checked for other conditions that affect your risk of transient ischaemic attacks and stroke such as:
- high blood pressure
- atrial fibrillation
- high cholesterol
- diabetes.
If you have any of these conditions, keep them under control.
Related websites
Stroke Foundation external link
Information about the causes, signs diagnosis and treatment of transient ischaemic attacks.
Clinical review
This content was written by HealthInfo clinical advisers. It has been adapted for Health Information and Services.